Dr. Ravi Nagar
Menu
Emergency? Call us!
+91 7869966988
+91 7869966988
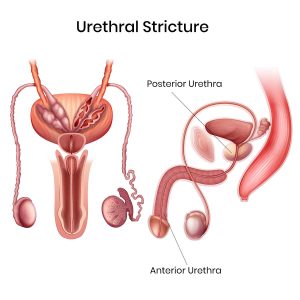
Urethral stricture disorder is a condition characterized by the narrowing or constriction of the urethra, the tube that carries urine from the bladder out of the body. This narrowing can obstruct urine flow and lead to a range of urinary symptoms and complications. Urethral strictures can occur at any age and may result from various causes, manifesting in different types and requiring diverse treatment approaches.
Age Groups:
Urethral stricture disorder can affect individuals of all ages, but it is more commonly diagnosed in men due to their longer urethra. In children, strictures are often congenital or result from trauma. In adults, the condition is frequently related to injury, infection, or previous medical procedures.
Causes:
Types of Urethral Strictures:
Investigations:
Surgery Types:
Conclusion:
Urethral stricture disorder presents with a variety of symptoms and can significantly impact urinary function and quality of life. Accurate diagnosis through imaging and endoscopic evaluations is crucial for determining the appropriate treatment. Management strategies range from minimally invasive procedures to complex reconstructive surgeries, aiming to restore normal urinary function and alleviate symptoms.